|
Malignant Melanoma - Patient Information
What is malignant melanoma and where does it develop?
Malignant melanoma is the most aggressive and life-threatening skin cancer. It develops in the cells that give the skin its color (melanocytes) and has a very high tendency to spread to other parts of the body. The cure rates depend greatly on the stage of melanoma by the time of detection. The earlier it is detected the better the chances of being cured. Therefore it is important to know what to look for and how to prevent it.
Who is at risk from malignant melanoma and how common is it?
Malignant melanoma occurs among all adequately studied racial and ethnic groups. The frequency of its occurrence is closely associated with the constitutive color of the skin, and depends on the geographical zone. Incidence among dark-skinned ethnic groups is 1 per 100,000 per year or less, but among light-skinned Caucasians up to 50 and higher in some areas of the world. The highest incidence rates have been reported from Queensland, Australia with 56 new cases per year per 100,000 for men and 43 for women. The current estimated annual incidence of melanoma in the United States among whites, adjusted for the same standard population and for the same year (1987) is 14 and 11. In Northern Europe the incidence is than 5 per 100,000 in countries of low insolation. Cutaneous malignant melanoma is the most rapidly increasing cancer in whites. The annual increase in incidence rates has been estimated to be between 3 and 7%, mortality rates increasing less quickly, though. These estimates suggest a doubling of rates every 10-20 years. The cumulative lifetime risk for melanoma is now in the order of 1 : 25 in Australia and it has been estimated to be around 1 : 75 in the United States by the year 2000. 1 out of every 105 American born in 1993 will develop malignant melanoma in his or her lifetime. In contrast, the risk in 1935 was only 1 in 1,500, in 1960 1 in 500, and in 1980 1 in 250. Malignant melanoma is now the forth most common cancer in Australia and New Zealand, the seventh most common in the USA and Canada, the tenth most common in Scandinavia and eighteenth most common in the United Kingdom. In contrast, for Africans and Asians the annual incidence rate of malignant melanoma is only 0.2 to 0.4 per 100.000 population, affecting mainly the palms, soles, and mucous membranes.
Figures from the U.S. suggest a statistically significant increase in thin tumours (<1mm) in all age groups except in men under 40 years of age. Thick tumours (>or=4mm) increased statistically significantly only in American males aged 60 years or older.
The male : female ratio is 1 : 1 in the U.S. and Australia. In Europe, the sex incidence shows a slight female preponderance in most countries. The sex ratio for incidence of melanoma varies with incidence: it is higher in females than in males in areas of low insolation and low incidence rates.
In contrast to NMSC, which mainly affects older individuals, the frequency of melanoma peaks in young people aged 20-45 years, although age-specific rates continue to rise with age. Approximately 50% of melanomas occur in individuals under 55 years of age. It is very rare prior to puberty, and when it does occur in children, about 50% of cases arise in giant congenital nevi.
Although we talk in general terms about the epidemiology of melanoma, this tumour has been subdivided into different tumour types. Some of these subtypes have different characteristics epidemiologically, both in incidence and mortality rates and also in factors likely to causation (e.g. sunlight exposure).
What causes malignant melanoma?
Environmental Factors
- Sun exposure: It has been reported that in areas with many hours of sunlight throughout the year, the occurrence of melanoma is the highest, leading to the conclusion that sun-exposure may be a risk factor in developing melanoma. There are also indications that skin that is not used to sun-exposure (such as the skin of office workers) has a higher tendency to develop melanoma when intensely exposed to UV radiation than skin that is continually exposed to sunlight (such as the skin of outdoor workers). A very important risk factor is exposure to the sun in childhood especially when there is a history of sunburn early in life. Even sunburn in adulthood seems to be related to the development of melanoma.
- Artificial UV sources: Several studies lead to the conclusion that artifical UV light may also be a melanoma related risk factor. Such light sources are mainly tanning beds which use high amounts of UVA.
- Socialoeconomic status: Several studies have reported that melanoma is more prevalent in those of high socioeconomic status. An explanation of this finding may be the fact that these people can better afford holidays in areas of high UV intensity, as well as expensive outdoor hobbies like sailing, which increase the risk of melanoma due to intense sun exposure.
Skin Type
The individual skin type (mainly skin type I and II) and the presence of multiple moles are important melanoma-related risk factors which should be taken into consideration when planning to expose yourself to UV-radiation. Therefore take preventive actions.
Genetic Factors
There seems to be evidence that a family history of melanoma in at least one first degree relative might increase the risk of developing melanoma. In approximately one third of melanoma patients there has been a genetically abnormality reported.
Some rare genetically determined disorders or skin diseases also exist which may increase the risk of developing malignant melanoma.
How to spot malignant melanoma
There are several criteria that may lead to the diagnosis of a malignant
melanoma. The most important one is the ABCDE-rule.
- A
- stands for assymetry. The mole or lesion is assymetric which means
no matter where you mirror the lesion it will not be equal.
 
- B
- stands for irregular borders. The mole or lesion has irregular borders.
  
- C
- stands for irregular colors. The mole or lesion is irregularly colored
ranging from light brown to dark brown, black, red, blue or white
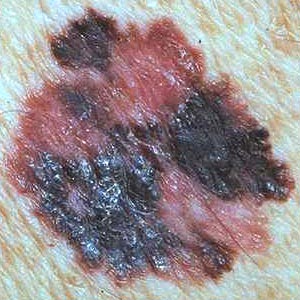
- D
- stands for diameter. A mole or lesion is suspicious if it is over 5 mm in diameter.

- E
- stands for elevation. The elevation of a mole or lesion may be
a hint for the lesion beeing malignant.
 
Patient history
If a lesion looks suspicious (see ABCDE-rule) the hint of a personal or family history of malignant melanoma may support an accurate diagnosis.
Dermatoscopy
This is a hand-held device used by dermatologists for close inspection of the top layer of the skin. It is absolutely painless. To get a better view the skin will be pretreated with oil in advance of inspection.
Biopsy
If there is still a doubt after all diagnostical tools have been used a biopsy will be advisable to state an accurate diagnosis. If there is a chance of malignant melanoma the lesion will be excised for further microscopic examination. This procedure will require a local anesthesia.
How does it occur?
Since malignant melanoma may lead to death and there are many different types and appearances, it is important to have a dermatologist take a look at a suspicious mole or lesion to catch melanoma at an early stage.
The appearance of malignant melanoma may vary from a flat patch to a nodule or wart-like lesion. Its color can range from red, brown, grey to black shades. It can appear anywhere on the human skin, from sun-exposed areas to the soles of the feet, palms of the hands, nails, genital and oral skin (mucosa).
At first it usually grows in a horizontal direction being rather superficial but depending on the type of melanoma it may start growing rapidly in a vertical direction at an early stage. If the melanoma is advanced it may start bleeding and ulcerate. The further developed a melanoma is the higher the risk of spreading to other parts of the body.
How to prevent malignant melanoma
According to the risk factors for malignant melanoma, the following preventive measures are recommended:
- UV exposure should be minimized. Prolonged sunbathing, especially of non-acclimatized skin, as well as the use of tanning lamps is not advisable. Children under three years of age should be kept in the shade.
- Sun protection should be achieved through adequate clothing. Broad-brimmed hats, shirts with long sleeves and sunglasses are recommended. Children should be especially carefully dressed when playing outside.
- The use of adequate sunscreens is recommended. This should not lead to prolonged sunbathing, though, thinking that all risks have been ruled out with the use of sunscreens.
- Sunburns should be avoided, especially in children.
If you already have several moles you should examine your skin regularly. Click here to see how to do a self exam. If you have a suspicious mole or spot seek the advice of a dermatologist.
- People with multiple moles, abnormal moles or a family history of melanoma should regularly have their skin checked by a dermatologist.
To learn more about preventive action klick here.
Is it really malignant melanoma?
There are many skin diseases that may look similar to MM. Just because you have a rough spot on your skin does not mean you have cancer, yet it is something that should be taken seriously. If you have noticed a strange looking area of skin please see your dermatologist or doctor.
What could go wrong?
Malignant melanoma may ulcerate and have a tendency for infection. Melanomas may also spread to other parts or organs of the body at an early stage (metastasize). Usually malignant melanoma metastasizes at first over the lymphatic system into the surrounding skin or into the regional lymph nodes. Later internal organs such as the lungs, liver, brain, and bones may be affected.
I have malignant melanoma what can I do?
Since malignant melanoma is the most dangerous and most life-threatening of all skin cancers you should seek the advice of a specialist and discuss immediate action and treatment options with him/her. But try to keep in mind that the choice of treatment depends on your individual situation. Different factors such as tumor size, thickness, and stage may be taken into consideration when chosing a treatment.
First choice of treatment is the surgical removement of the tumor. This treatment will require a (local) anesthetic. Usually not only the tumor is cut out but also a security margin of 1 cm (horizontally and vertically) will be removed to make sure no diseased tissue is overlooked.
If the tumor has already reached the lymphatic system, a surgical removal of the whole lymph node may be required to minimize the risk of the melanoma spreading to other parts or organs of the body.
If the melanoma has already spread to other body organs (eg. brain, liver) these tumors should also be removed if possible. If surgery is impossible, radiotherapy or chemotherapy might be suitable treatments.
Radiotherapy
This therapy uses X-rays to destroy damaged cells. Usually the affected area needs to be treated several times to reach a dose that is effective, depending on the size and stage of the tumor. Therefore the therapy might last several weeks.
Chemotherapy
This kind of treatment uses chemicals that have a specific toxic effect upon cancerous tissue. Most anticancer drugs are administered into the vein or into muscle, a few are swallowed. Chemotherapy is usually given in cycles: a treatment period is followed by a recovery period, then another treatment period follows, and so on. There are several chemotherapeutic substances available. Individual factors such as tumor spread, affected organs and the patient's general health determine the choice of therapy.
Immunotherapy
Immunotherapy is a therapy that helps to support the immune system. Usually the drug called interferon alpha or interleukin-2 is injected underneath the skin. This treatment might last quite a long time (up to a year or even longer) and is often used in combination with surgical removal of the tumor, radiotherapy or chemotherapy. Unfortunately this therapy is connected with several disturbing side effects e.g. flu-like symptoms such as fever, drowsiness and nausea. Sometimes it may also cause a reduction of white, sometimes even red blood cells
This listing of possible treatment options does not claim to be complete. Besides established treatments it includes experimantal chemo- and immuno(chemo)therapies which are being applied in specialized centers and whose efficacy is still being investigated.
Dealing with skin cancer can be very frightening therefore seek the advice of a dermatologist whom you trust and discuss every aspect of your disease openly with him/her.
What are the chances of being cured?
There are several factors on which the prognosis for malignant melanoma is based.
Tumor thickness
The thickness of a melanoma is measured in milimeters from the top layer of the tumor to the deepest invasive melanoma cell. Melanomas less than 0.75 mm thick present only a low metastatic risk, wheras tumors of 3 mm or more in thickness present a very high risk.
Levels of invasion
These criteria are based on the depth of penetration into the layers of the skin and range from level one (tumor cells in the epidermis) to level 5 (tumor cells below the dermis). The 5-year survival rate decreases with level. Level 1 or 2 has a survival rate of over 90%.
Localization
Melanomas on the extremities have a better prognosis than those on the head or the trunk. Melanomas in the genital region have a poor prognosis, as they are often discovered at a late stage.
Gender
Women statistically have a somewhat better chance of survival than men.
Other factors
The tendency to ulcerate, the presence of tumor cells in blood vessels and the cell activity of the tumor cells are also factors which are helpful in making a prognosis.
No matter what your personal prognosis might look like donīt let cancer beat you. It is not a death sentence. Nowadays there are several effective treatments available to keep fighting skin cancer!
|